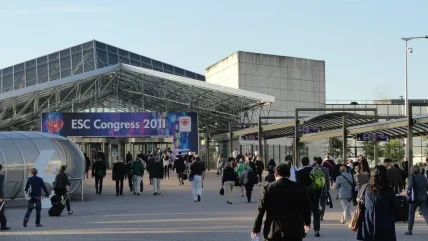
The European Society for Cardiology (ESC) is an international body that aims to bring together healthcare professionals from around the world. Its aim is to help those working towards increasing living standards, promoting healthy lifestyles and ultimately helping people live longer.
Its annual congresses are an opportunity for the scientific community to share its research and findings into cardiovascular health and well-being and to provide a foundation for greater understanding. They also help shape future research studies and guide policymakers, governments and organisations. Below we take a look at some of the findings related to diet.
Do fat guidelines need revisiting?
A study of more than 135,000 people from 18 low, middle and high-income countries was presented to the congress. The research looked at fat intake, and its impact on cardiovascular health and mortality.
The work, which was part of the Prospective Urban-Rural Epidemiology (PURE) study, led the team of scientists behind it to call for a reconsideration of global dietary guidelines in light of the new data presented. They said high carbohydrate intake was linked to worse total mortality and non-cardiovascular (CV) mortality outcomes, while high fat intake was associated with lower risk.
The research looked at the dietary habits of 135,335 individuals, aged 35–70, from countries in North America and Europe, South America, the Middle East, South Asia, China, South East Asia and Africa. Data for the consumption of carbohydrate, total fat and types of fat was captured on a country-by-country basis and married with mortality figures and other health-related conditions.
“Our findings do not support the current recommendation to limit total fat intake to less than 30% of energy and saturated fat intake to less than 10% of energy,” said study investigator Dr Mahshid Dehghan from the Population Health Research Institute, McMaster University, in Hamilton, Ontario, Canada.
During the study period, 5,796 deaths – of which 1,649 were related to CV – were recorded and 4,784 major CV events over a median follow-up of 7.4 years. Researchers concluded carbohydrate intake in the highest versus lowest quintile was associated with a significant 28% increased risk of total mortality. However, total fat intake in the highest versus lowest quartile was associated with a significant 23% reduction of total mortality risk, an 18% reduced risk of stroke, and a 30% reduced risk of non-CVD mortality.
“Limiting total fat consumption is unlikely to improve health in populations, and a total fat intake of about 35% of energy with concomitant lowering of carbohydrate intake may lower risk of total mortality. In fact, individuals with high carbohydrate intake, above 60% of energy, may benefit from a reduction in carbohydrate and increase in the consumption of fats,” Dehghan said.
The study highlighted different types of fat with a ‘significantly’ reduced mortality risk. It was 14% lower for saturated fat, 19% for monounsaturated fat, and 20% for polyunsaturated fat. Higher saturated fat intake was also associated with a 21% decrease in stroke risk.
Speaking of the study itself, Dehghan said, “PURE provides a unique opportunity to study the impact of diet on total mortality and CVD in diverse settings, some settings where over-nutrition is common and others where under-nutrition is of greater concern.”
Planting the seed
The same PURE study concluded that eating even a “relatively moderate” intake of fruit, vegetables and legumes such as beans and lentils may lower a person’s risk of cardiovascular disease (CVD) and death. The study, which was presented at the congress and published in The Lancet, used country-specific food frequency questionnaires.
For this element of the research, scientists assessed associations between fruit, vegetable, and legume consumption at baseline, and risk of CVD and mortality after a median of 7.4 years of follow-up. They found greater fruit, vegetable, and legume intake was associated with lower total mortality, and non-CV mortality.
“To our knowledge, this is the first study to report on the associations of fruit, vegetable and legume intake with CVD risk in countries at varying economic levels and from different regions,” said Dr Andrew Mente, also from the Population Health Research Institute, McMaster University.
“Previous research, and many dietary guidelines in North America and Europe, recommended daily intake of these foods ranging from 400–800g a day, but this is unaffordable for many people in low to middle-income countries,” he explained. “Our findings indicate that optimal health benefits can be achieved with a more modest level of consumption, an approach that is likely to be much more affordable.”
Other notable findings were that three to four servings a day were just as beneficial as greater amounts, and the preparation of vegetables was a contributing factor.
There was a lower risk of CVD and death with raw versus cooked vegetable intake, but raw vegetables were “rarely eaten in South Asia, Africa and South East Asia”, according to Mente.
“Since dietary guidelines do not differentiate between the benefits of raw versus cooked vegetables,” he continued, “our results indicate that recommendations should emphasise raw vegetable intake over cooked.”
A team from the National Institute for Health and Welfare in Finland presented their findings to a 12-year study involving 4,000 subjects looking at the impact of high levels of salt intake. It concluded the risk of heart failure doubled with an increased consumption of sodium chloride.
“High salt intake is one of the major causes of high blood pressure and an independent risk factor for coronary heart disease (CHD) and stroke,” said Pekka Jousilahti, research professor at the National Institute for Health and Welfare.
“In addition to CHD and stroke, heart failure is one of the major cardiovascular diseases in Europe and globally, but the role of high salt intake in its development is currently unknown.”
The research team said the study was intended to look at the relationship of salt intake and the development of heart failure.
“Estimation of individual salt intake is methodologically demanding and therefore suitable population-based cohorts are rare,” it said.
The study used a sodium extraction over 24 hours, said to be the ‘gold standard’ for salt intake estimation at individual level.
“The heart does not like salt,” said Jousilahti. “High salt intake markedly increases the risk of heart failure. This salt-related increase in heart-failure risk was independent of blood pressure.
"People who consumed more than 13.7g of salt daily had a two times higher risk of heart failure compared with those consuming less than 6.8g.
“The optimal daily salt intake is probably even lower than 6.8g. The World Health Organization recommends a maximum of 5.0g a day and the daily physiological need is 2.0–3.0g.”
Go high to stay low
A study of nearly 20,000 subjects found that higher coffee consumption was associated with a lower risk of death. The observational research project concluded that the drink could be included as part of a healthy diet.
The cohort was of Mediterranean origin and all middle-aged. The study was conducted within the framework of the Seguimiento Universidad de Navarra Project, a long-term prospective cohort study in more than 22,500 Spanish university graduates that started in 1999.
Subjects were followed for around a decade, during which 337 died. It was determined that those who consumed at least four cups of coffee a day had a 64% lower risk of all-cause mortality than those who never, or almost never, consumed the drink. There was a 22% lower risk of all-cause mortality for each two additional cups a day.
“Coffee is one of the most widely consumed beverages around the world,” said Dr Adela Navarro, a cardiologist at Hospital de Navarra, Pamplona, Spain.
“Previous studies have suggested that drinking coffee might be inversely associated with all-cause mortality but this has not been investigated in a Mediterranean country.”